Mae’r cynnwys hwn ar gael yn Saesneg yn unig.
Research suggests that these changes may increase a person’s likelihood of developing a mental health condition. What does this mean exactly?
The cells in our brains, known as neurons, are all connected in a complicated network. Across our lifetime, new connections are formed, old connections are lost, and existing connections are strengthened or weakened.
Throughout childhood, these connections are continually created and modified.
For a child to develop skills such as crawling, walking, and talking, the brain must sprout millions of new cells, with each individual cell connecting with thousands of other cells over time.
As a child matures, many of these connections are modified or removed until an advanced, resourceful brain is formed. These processes continue (although at a much slower rate) throughout our adult lives, allowing us to learn from our experiences across the lifespan.
The ability of a child’s brain to change is hugely beneficial, as it allows development to occur at an incredible rate. However, to do this, the young brain must be extremely sensitive to events occurring within its environment.
As well as increasing the brain’s potential to learn, this heightened sensitivity increases the vulnerability of the brain to stressful life events. Such events are commonly referred to as adverse childhood experiences (ACEs) and may include physical abuse, emotional abuse, neglect and exposure to domestic violence.
Adverse childhood experiences: the risks
Simply put, individuals who have experienced a number of ACEs seem to be at a higher risk of developing mental health conditions such as depression, anxiety and substance abuse.
Although there are many reasons behind this increased risk, one could be the physical impact stressful events have on the brain.
If a person is in a constant state of fear or stress, their brain may adapt to survive within this environment.
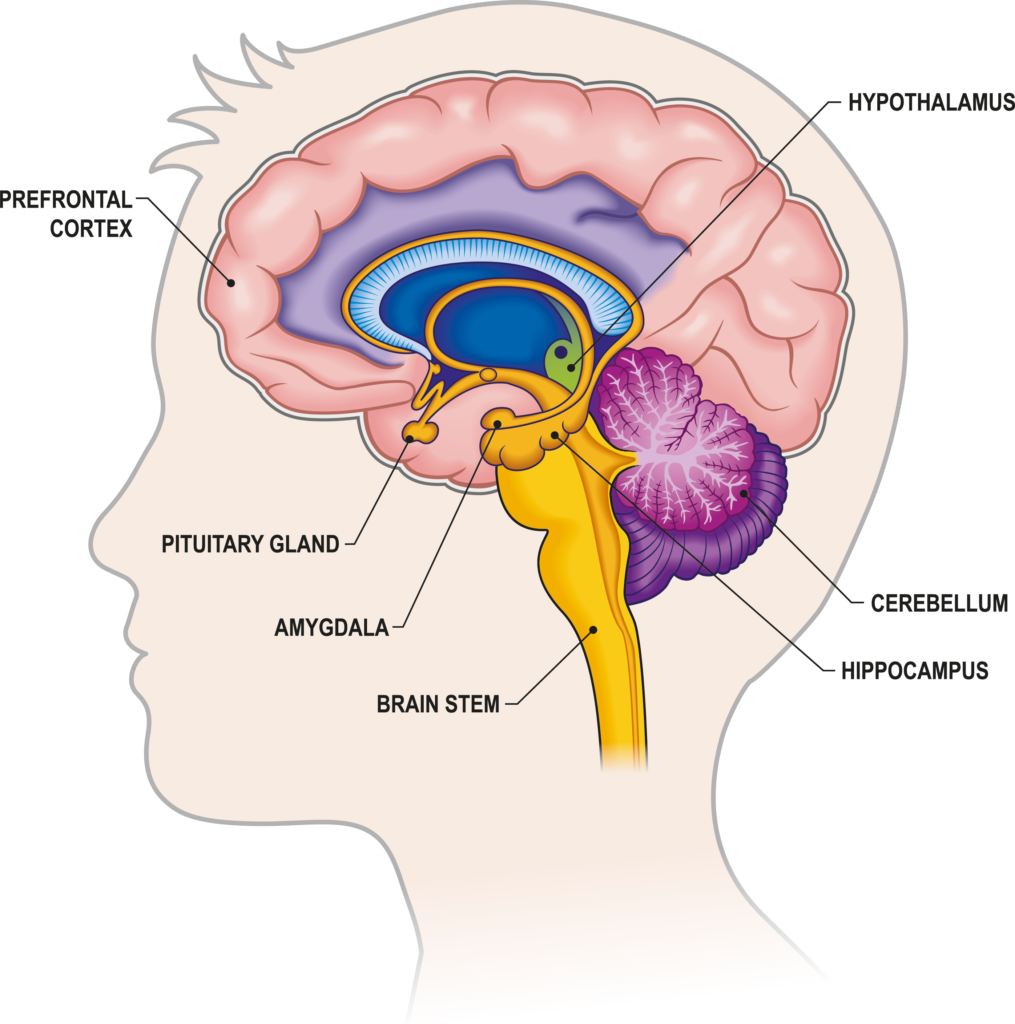
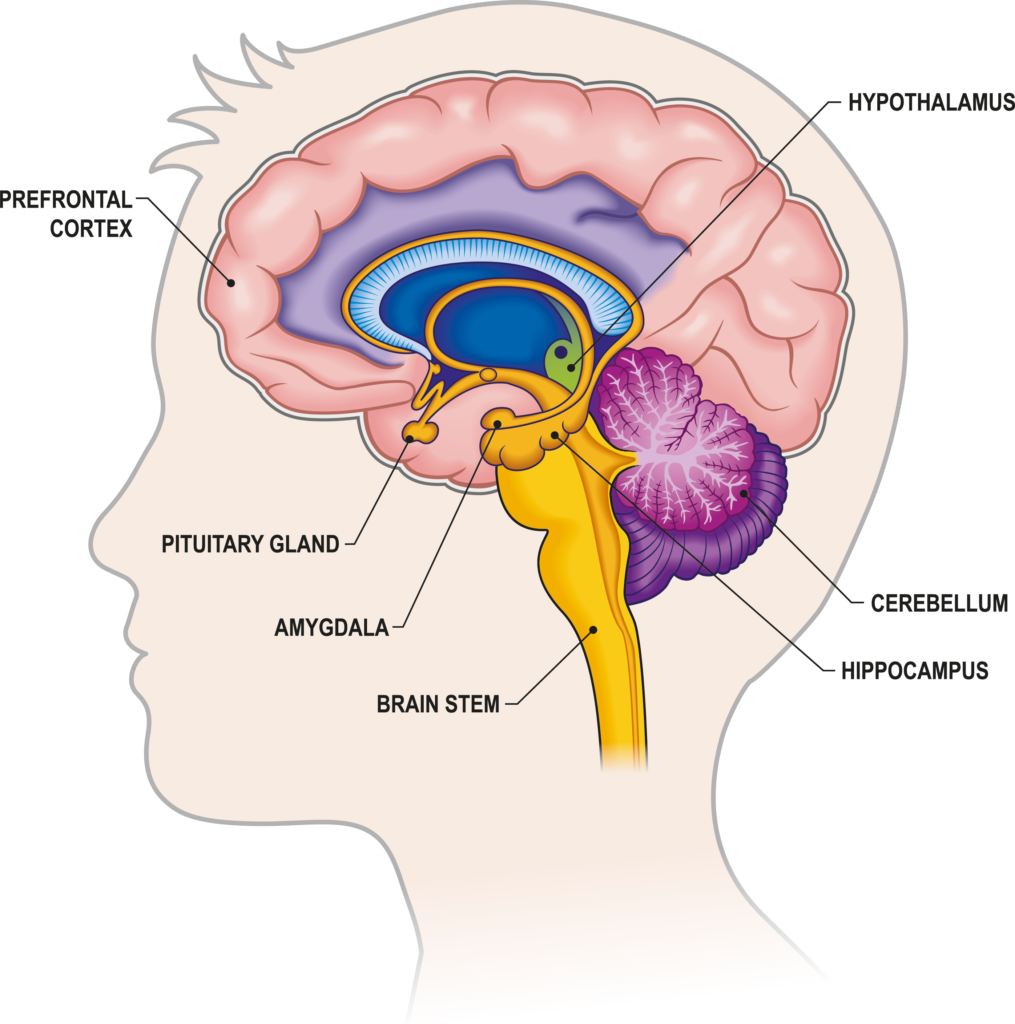
This may lead to impaired development of areas of the brain involved in logical thinking (such as the prefrontal cortex) and memory (such as the hippocampus).
On the other hand, areas involved in emotional responses (such as the amygdala) become more active, resulting in that person becoming more vigilant to threatening information.
Together, these changes may result in difficulties in regulating emotions, making decisions, and managing stress. But, how?
The consequences of the brain’s coping mechanisms
Firstly, imagine walking down an unfamiliar street at night. You may hear a noise in the distance and immediately become on edge. You may quickly realise that the noise came from a nearby cat, and begin to rationalise your response.

This initial response of being ‘on edge’ is due to the amygdala: a small, almond-shaped structure deep within the brain.
It is critical in generating emotional responses, particularly to a threat. When presented with a potential threat, the amygdala undergoes a surge of activity, which may result in the generation of a ‘fight or flight’ response.
The rationalisation that follows is due to the prefrontal cortex (PFC), which is positioned behind the forehead. It is essential in decision making, rule learning, and social behaviour.
It is often described as the “CEO of the brain”, as it is able to regulate many brain regions, including the amygdala.
When we are presented with a potential threat, the PFC can decide whether a response from the amygdala is justified and regulate its activity accordingly.
So, back to our dark street. If the activity of the PFC is impaired (for example, after a period of intense stress), there is reduced regulation over the amygdala and reactions to potential threats may become more intense and longer-lasting.
Instead, you may hear a noise in the dark street and have difficulties rationalising it. You may become incredibly anxious and fearful. You may begin to remember events that were similarly threatening.
In this way, it becomes clear to see how these changes to the brain may result in a predisposition to mental health conditions such as anxiety and depression.
Are these changes permanent?
Although it is important to bear these possible changes in mind, they are not inevitable. Whether such events impact a person depends on their genetics and their environment.
For example, a person may experience a number of ACEs but have genes that make them more resilient to stressful events.
They may also have a supportive family, close friends, and a variety of hobbies or interests. These are referred to as protective factors and can prevent the development of mental health conditions.

Moreover, should changes occur, they are not irreversible. The brain has the potential to change and adapt throughout childhood and adulthood so the areas that may have been affected by certain events can be strengthened over time.
For example, exercise, socialising, and mindfulness exercises have all been found to strengthen frontal areas of the brain, including the PFC.
Moreover, the PFC’s functioning can be optimised through self-care, such as having plenty of sleep and avoiding excessive drug and alcohol use.
Read more:
- NHS UK – ACEs
- Maryland Coalition of Families – ACEs